What's New
How Genetics Influence Opioid Pain Medications

How Genetics Influence Opioid Pain Medications
The Role of Genetics in Opioid Pain Relief and Effectiveness
What Are Opioids & When Are They Prescribed?
Opioid medications are commonly used to treat or prevent pain in different circumstances. Pain treated with opioids is usually at least of moderate severity (or predicted to be, if untreated). Opioids are sometimes used for other reasons, depending on the specific medication and circumstance.
Opioids are usually intended to manage short term pain needs, like after surgery or dental procedures, or for injuries that cause considerable pain. Opioids are also needed to help many individuals manage cancer pain, and duration of use can exceed typical use in those without cancer. It should also be noted that a small portion of individuals with long-term chronic pain not due to cancer may also rely on opioids, typically when other treatments have not been adequate in managing their pain. Opioids do have important risks associated with them, so use in any scenario is done after careful professional evaluation of both risks and benefits.
It is also important to note that opioids, at their best, may only partially manage pain. In particular, this tends to occur in those with more severe pain. This is why reducing pain to the point that someone can carry out aspects of their normal life is usually a realistic goal, rather than eliminating pain entirely.
Risks can range from constipation, dry mouth and dizziness to the development of
dependence. Accidental overdose (e.g., individuals forgot they already took their dose, then take it again as a result) is a particular concern. When exposed to greater doses of opioids, breathing can become more difficult, and unfortunately, some individuals may pass away. In recent years, antidote accessibility, as well as awareness and education surrounding opioid overdose, have increased in multiple places.

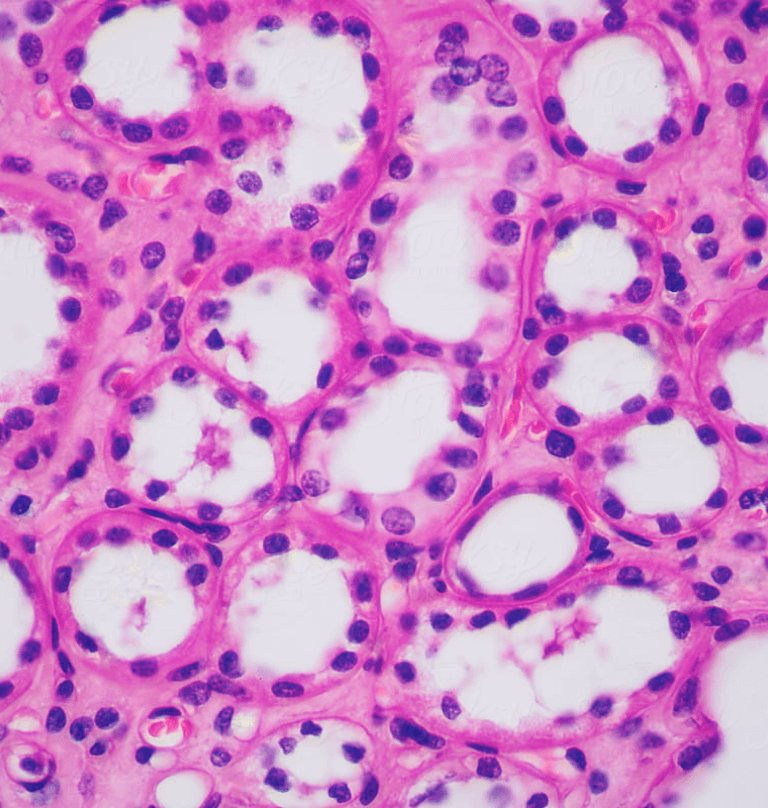
Why Opioids Work Differently for People
Opioids can work differently across individuals for several reasons. For some, the underlying cause of the pain may not be addressed by the effects of opioids. Opioids are generally effective when tissue or nerve injury generates pain signals that are transmitted through the nervous system. Opioids work by attaching to members of a family of "receptors" that are present on the surfaces of cells. This causes a chain reaction that ultimately calms the delivery of this pain signal for those in need. For some pain sufferers, the cause of their pain doesn't involve this process, and so opioids don't usually work very well.
In some people, longer term use of opioids can cause adaptations in the body which essentially "re-wire" an aspect of the nervous system, causing opioids to no longer work as they once did.
The functioning of key organs responsible for processing and eliminating opioids from the body also have an impact. For those with reduced kidney and/or liver function, opioids and their byproducts may accumulate in the body, impacting both the effectiveness and toxicity of the medication.
Age and presence of other medical conditions often impact side effect risk. For example, older individuals tend to be more prone to dizziness and confusion as a result of taking opioids. Another example would be those that experience asthma. These individuals tend be more at risk of experiencing the breathing side effects (as discussed earlier).
Biological sex at birth also influences how opioids work in the body for a variety of reasons.
Interactions between opioids and certain other medications taken at the same can also change the opioid's effectiveness, as well as worsening some safety risks.
It is also important to note that different opioids may produce different effects in the same individual. This could be due to several reasons, including the potency of the specific opioid, the preference of the specific opioid to member(s) of the "receptor" family (as mentioned earlier), and differences in the way they are metabolized compared to one another. In fact, differences in metabolism contribute both to why the same person may respond differently to different opioids and to why two otherwise similar people may respond differently to the same opioid and dose. This is often due in no small part to genetics.
The reasons above can inform precautions and warnings associated with the medications (e.g., tramadol contraindications).
The Genetics Behind Opioid Metabolism
A few key opioids are metabolized, at least in part, by an enzyme called CYP2D6. This
enzyme is found, in particular, in the liver and also helps metabolize about a quarter of all medications.
The "version" of CYP2D6 found in your liver depends highly on your DNA. In short, variations in this gene (also known as CYP2D6) influence how your body metabolizes certain opioids. Depending on how "slow" or "fast" your version is, your ability to benefit from the medication while experiencing less significant side effects can differ greatly from the next person.
How Metabolism Impacts Opioid Effectiveness
Some opioids require CYP2D6 metabolism to "activate" them in the body before experiencing any effect (i.e., tramadol and codeine metabolism, respectively). This means that sluggish or slower versions of CYP2D6 may explain why some people feel that tramadol or codeine is not working.
On the other hand, those with "overactive" versions of CYP2D6 tend to activate too much of the dose. This means that they may have inadvertently taken a greater dose than intended. As a result, side effects tend to be worse, and, depending on some of the non-genetic factors already discussed, may cause significant harm.

Common Opioids Impacted by Your Genes
Beyond codeine and tramadol, the opioid hydrocodone can have some overlapping risks. In brief, in those with "slow" versions of CYP2D6 may be encounter less benefit because it too must be activated. However, this tends to be a lesser issue compared to codeine and tramadol, and those with faster or more active versions of CYP2D6 do not appear to be impacted by their hydrocodone metabolism [1] . It should be noted, however, that depending on where you live, hydrocodone may not be used to treat pain.
A newer IV opioid called oliceridine (brand name: Olinvyk) used for short term pain is also metabolized by CYP2D6. However, those with very slow versions are at higher risk of side effects, and this could mean that the health care team needs to increase monitoring and the time interval between doses.
Fentanyl, when given IV/IM after surgery is metabolized by a different enzyme called
CYP3A4. Certain variations in the underlying gene suggest that some could benefit from lower doses.
Oxycodone is also metabolized (in part) by CYP2D6. Though we know that variations in CYP2D6 can impact oxycodone metabolism, it doesn't seem to have an impact on oxycodone side effects or effectiveness. This is likely because the medication byproduct formed when metabolized seems to act somewhat similarly to oxycodone itself.
How Genetic Testing Can Improve Opioid Pain Management, and,
How Inagene Supports Personalized Opioid Treatment
Pharmacogenetic testing can help predict risk of side effects and lack of effect based on the descriptions above. This means that instead of taking these medications without having been tested first (and having to experience unmanaged pain or problematic side effects), the chance of a better outcome right from the start can increase.
Furthermore, Inagene's tests also include other medications used to treat various types of pain, including those that might complement or even reduce the need for opioids. This includes the medications celecoxib, ibuprofen and carbamazepine.
Ultimately, Inagene's tests help your health care teams put in place personalized pain management when managing your needs. This also means that genetic testing for pain medications is now a reality.
This website has been developed by Inagene Diagnostics Inc for information purposes only. It does not provide medical advice, diagnosis, treatment or care. If you have a health problem, medical emergency, or a general health question, you should contact a physician or other qualified health care provider for consultation, diagnosis and/or treatment. Under no circumstances should you attempt self-diagnosis or treatment based on anything you have seen or read on this website. For more information about how to use this site, please see our Terms of Service.
References